CISM / Peer Support
Standing Together
Before, During,
& After a Crisis
First Responder Therapy Dog Rocket AKC THDX
Peer Support: Standing Together, Before the Crisis
First Responder Peer Support is built on one simple truth — those who serve best understand those who serve. Peer Support connects trained responders with their fellow professionals to provide understanding, encouragement, and practical help through life’s challenges. Whether it’s stress from the job, family strain, or the cumulative impact of critical incidents, peers offer a safe, confidential space to talk with someone who “gets it.” Peers are the first line of support when the load gets heavy.
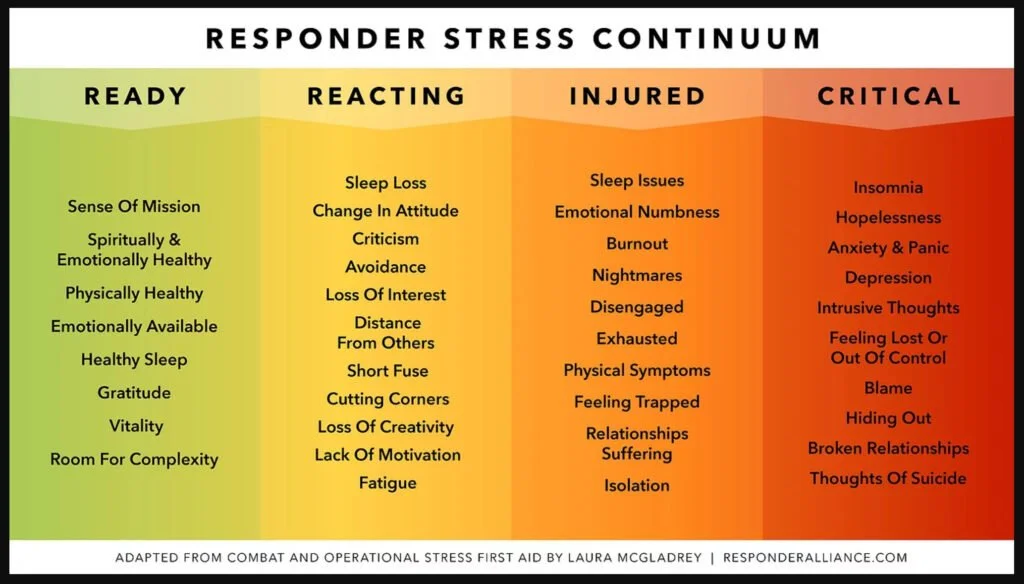
While Critical Incident Stress Management (CISM) is an essential tool used after a traumatic event to help responders process what happened, Peer Support is about connection long before the crisis. It’s the quiet check-in after a tough call, the cup of coffee shared in silence, or the text that simply says, “You doing okay?” These small moments of care build the resilience that keeps our people healthy and ready to serve.
Every agency in N. Idaho has its own version of Peer Support and it’s important to know what resources are available where you work. Your trained Peer Supporters know what’s available and will walk the road to wellness with you willingly and confidentially. Whether you’re reaching out for help or thinking about joining a Peer Support team, remember — you don’t have to carry the weight alone, and you might be the reason someone else doesn’t have to either.
About the CISM Process
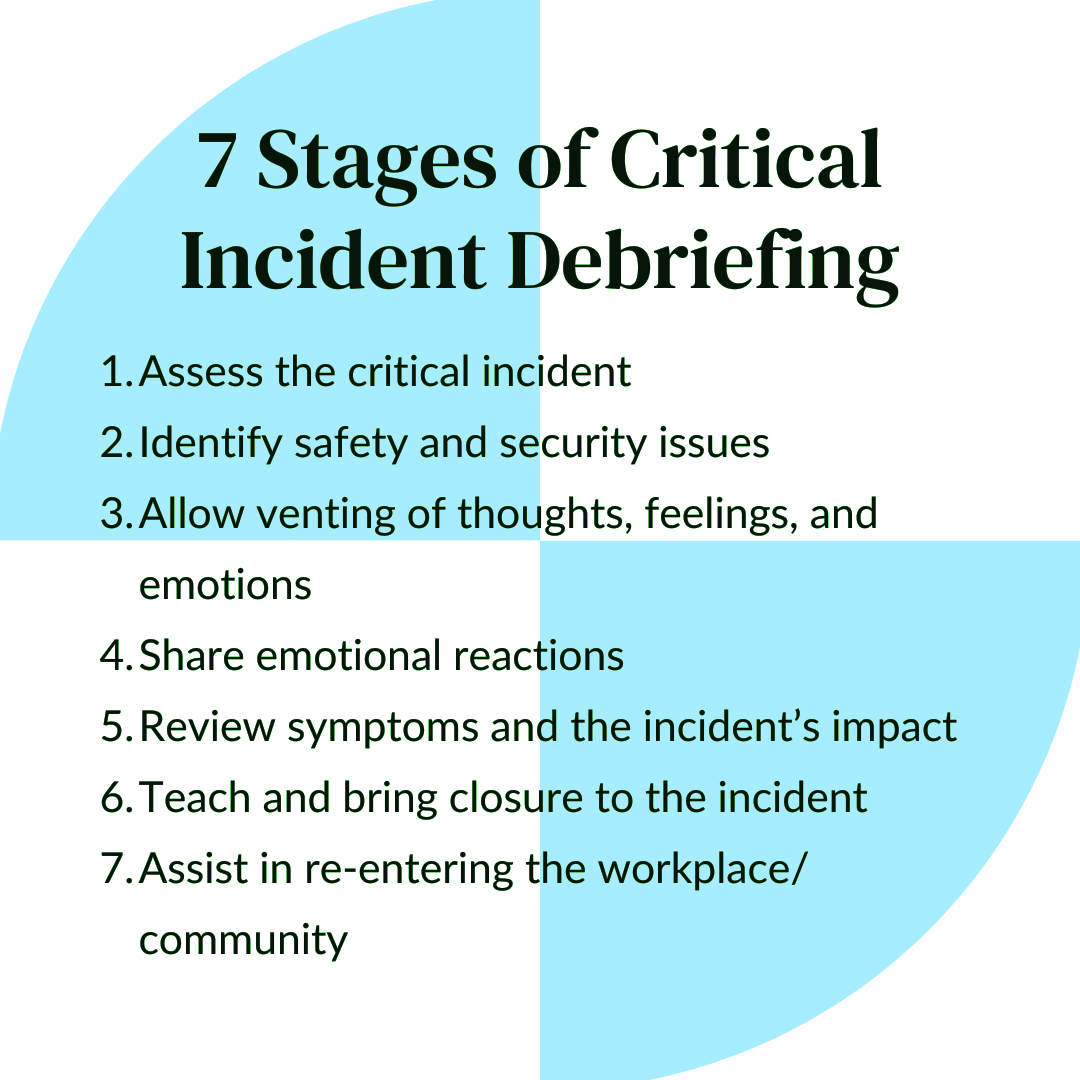
A Critical Incident Stress Management (CISM) debrief with first responders, led by a clinician, chaplain and a peer support team member, typically follows a structured, multi-step process designed to address emotional reactions and promote psychological well-being.
The first step is an introduction where the clinician explains the purpose of the debrief, ensuring a safe, confidential space for participants. Next, the participants identify their role in the event and often will share their position in the department. The third step involves individual sharing, where responders describe their experiences, thoughts, and emotional reactions to the incident.
The clinician normalizes their responses and validating their feelings. The pieces of the incident are gathered from the participants and made into a clear picture where the brain has an opportunity to process. The fourth step focuses on education, where the clinician explains common stress reactions, both immediate and delayed, that may occur after such traumatic events. Then, the clinician provides coping strategies and resources for continued support.
The debrief ends with a closing, ensuring participants know how to access additional mental health resources and reminding them of the importance of self-care and peer support. The clinician’s role is to facilitate a healing environment and offer tools for resilience.
We’ve Got You Covered
Each of our Clinicians covers a county. Find your lead clinician below and reach out to them directly.
Bonner County
Linda Leonard
Boundary County
Linda Leonard
Kootenai County
Nicole Nestor-Gray
Diana Kelsey
Lindsey Petrick
Preston Herdt
Benewah County
Natalia Sole-Pedrosa
Shoshone County
Nicole Nestor-Gray
Natalia Sole-Pedrosa